The Alliance for Health Policy and Systems Research works to improve the health of those in low- and middle-income countries (LMICs) by supporting the generation and use of evidence that strengthens health systems.
As an international partnership hosted by the World Health Organization, we work together with organizations around the world.

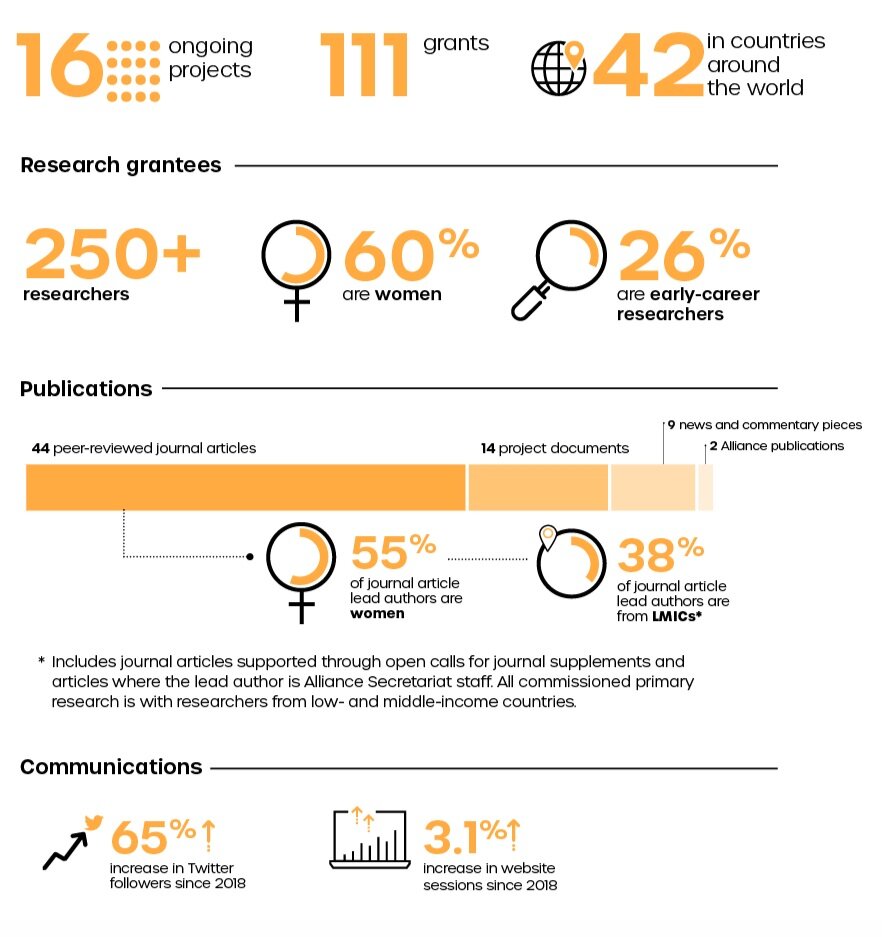
2019 by the numbers
* Most figures based on those grantees that responded to the annual survey
Where we work
Message from the Board Chair
2019 was a year of considerable progress in science and public health – and in the field of health policy and systems research (HPSR). The Alliance has been a key driver of this, and this annual report is a testament to that.
The Alliance has led the way in identifying research priorities for the next decade. Whether the focus is on primary health care systems, achieving the health-related sustainable development goals (SDGs) or understanding how health systems can support the health and well-being of migrants, the Alliance has supported important publications this year that set a clear path for the future.
In 2019, the Alliance also continued to make a strong case for the field. Working with core partners through the Learning, Engaging and Advocating for HPSR (LEAP) Forum, the Alliance has been advocating for more locally-driven research in low- and middle-income countries (LMICs), where it can have an outsized impact.
The Alliance has been investing in the future, too. Its programmes to strengthen the capacity of early-career researchers and programmes to institutionalize embedded research are laying important groundwork for the field.
Despite this progress, it is impossible to ignore growing challenges. We have seen a rise in public protests over inequity, corruption and lack of political voice, but also populist movements that are fueled by fear, distrust and division. Issues like climate change conflict and forced migration have continued to demand our attention, along with the evolving epidemics of non-communicable diseases, nutrition transitions, injuries, emerging infections and antimicrobial resistance.
HPSR is needed more than ever to seek ways of addressing health inequities and vulnerable populations. We need to use systems methods to better link research and action on health to the broader issues affecting people’s health and well-being.
The Alliance has played a leading role in developing the field of HPSR and in tackling these emerging challenges and is on a strong footing to continue to do so. This would not be possible without the oversight and guidance from the Alliance Board and Scientific and Advisory Committee (STAC), and I would like to thank my colleagues for their ongoing stewardship of the Alliance. The Secretariat and its executive director, Dr Abdul Ghaffar, have been a strong driver of change, and I look forward to seeing how they steer the conversation in the next decade
– DAVID PETERS
Message from the Executive Director
The Alliance’s core mandate is strengthening health systems in low- and middle-income countries (LMICs) by supporting the generation and use of research. As this year’s annual report shows, we do this by convening key stakeholders, strengthening capacities, investing in cutting-edge research and supporting policy-makers to incorporate evidence into their decision-making processes.
2019 was the fourth year of our current five-year strategic plan. As we start planning for the next period, we have commissioned an external evaluation of the Alliance and have already initiated dialogues with key individuals.
One thing that is already clear are the significant changes and transitions around the world: changes in the climate, changes in societies and politics, and changes in health systems themselves. These shifts require us to think beyond the six traditional building blocks of health systems. Therefore, in 2019 the Alliance kick-started discussions about broadening the span and scope of HPSR and working to redefine the boundaries of the field.
To do this, we are using some of the core approaches and tools from HPSR, such as systems thinking, and applying them to new areas. We are collaborating with colleagues across WHO to test how the use of systems thinking and HPSR can contribute to health systems strengthening while dealing with rehabilitation, road safety, health promotion and creating healthy environments. Our collaborations support the generation of local knowledge and its application for improved policies and decision-making.
We also firmly believe that determinants of health are strong drivers and predictors of health and well-being, and we are, therefore, supporting our WHO colleagues in the Eastern Mediterranean Region on a regional Commission on Social Determinants of Health.
I have no doubt that in 2020 we will continue to push the boundaries of HPSR. We look forward to wider discussion and debate, and we expect that our next flagship report on ‘learning health systems’ later in the year will be a big contributor to those deliberations.
– ABDUL GHAFFAR
We work
together.
Building the field of health policy and systems research requires an enthusiastic community of practitioners who have the opportunity to interact and share ideas.
Convening networks and spaces for sharing is an important part of what the Alliance does. This would not be possible without working closely with partners, both inside the World Health Organization and beyond.

Bringing people together
In 2019:
Learning, Earning, Engaging, and Advocating for HSPR (LEAP) Forum
“By investing at the district level and in the research institutions and supporting what we think of as rigorous questioning – it leads to a culture change. [...]That’s what makes a resilient system.”
— LOLA ADEDOKUN, Director of the Africa Health Initiative
Doris Duke Charitable Foundation
(Said during the UNGA74 side event,
UHC: Unachievable without evidence)
— LOLA ADEDOKUN, Director of the Africa Health Initiative
Doris Duke Charitable Foundation
(Said during the UNGA74 side event,
UHC: Unachievable without evidence)
The LEAP Forum is an important opportunity for the Alliance and its partners to advocate for the field of health policy and systems research. The Forum held an annual meeting in April of 2019, where a new structure and strategic focus for the Forum were agreed. A major activity for the Forum was holding a side event at the 74th United Nations General Assembly called ‘Universal health coverage: Unachievable without evidence’. The event was co-hosted by the Alliance and Health Systems Global (HSG) with support from the Government of Georgia. Representatives from the Doris Duke Charitable Foundation and UNICEF (all LEAP partners) were on the panel. Key issues raised included the need for investing in on-going learning for health initiatives, investing in local research capacity and promoting a culture of evidence use at all levels of health systems.
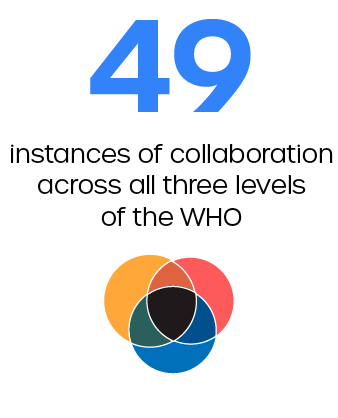
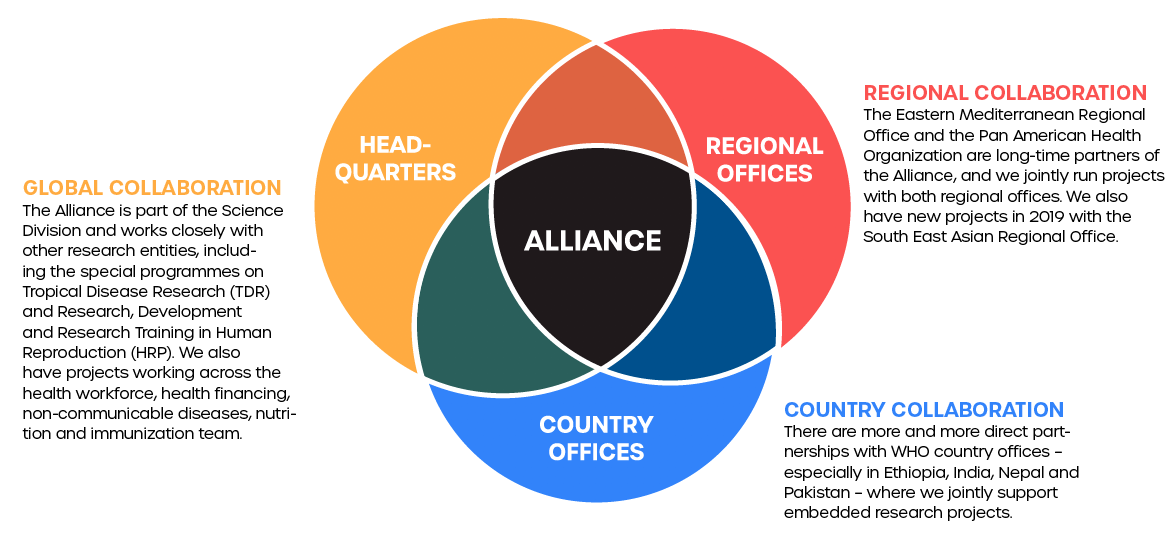
Partnering with the World Health Organization
Collaborating with others at headquarters and in the regional and country offices is critical for ensuring our work responds to the needs of those in LMICs.
This has been a year of transformation for the World Health Organization, and that has had an impact on the Alliance. We moved into the newly created Science Division in May 2019. As a cross-cutting division designed to support the evidence needs across the organization, moving into the Science Division has empowered the Alliance to collaborate more widely across all three levels of the organization.
For example, the Alliance has been working with TDR and HRP, under the stewardship of the Chief Scientist, to undertake a programme of work on Country-led Implementation Research for Universal Health Coverage. The project responds to requests from member states and provides support for implementation research projects on topics that countries prioritise as important for the achievement of UHC. In 2019, we worked with India, Ethiopia and Nepal.
In addition to collaborations with others at WHO Headquarters, we have also been working with several regional and country offices. For example, with the Eastern Mediterranean Regional Office (EMRO), we launched a new Commission on Social Determinants of Health chaired by Sir Michael Marmot, and we also established a regional learning platform for the Sustainable Development Goals (SDGs). Our embedded research projects on the health-related SDGs are done in collaboration with TDR and the Pan American Health Organization (PAHO).
We empower leaders.
Developing effective health systems requires sufficient capacity not only for delivering health services, but also for generating and using evidence to drive improvements in health systems.
Our focus is on ensuring local capacity for research production and update in LMICs, both at the individual and institutional levels. We specifically aim to increase participation in the field by historically under-represented groups. We also want to ensure appropriate systems and structures are in place to ensure close collaboration between researchers, policy-makers and implementers, and communities and citizens who access health services.

Empowering leaders
In 2019:
Mentorship programme for early-career women researchers
"An enriching learning experience. I'm so grateful."
— DR IJEOMA OKEDO-ALEX
Federal Teaching Hospital Abakaliki, Ebonyi State, Nigeria
Mentee participating in the Alliance’s publication mentorship support initiative after having her article published in BMJ Open
— DR IJEOMA OKEDO-ALEX
Federal Teaching Hospital Abakaliki, Ebonyi State, Nigeria
Mentee participating in the Alliance’s publication mentorship support initiative after having her article published in BMJ Open
Getting on the academic publishing ladder is an important step for emerging researchers. However, there is a gender gap when it comes to publishing and participating in research. To help redress this imbalance, the Alliance established a mentorship scheme for early-career women researchers working in the field of health policy and systems research.
Ten mentees from LMICs were paired with appropriate mentors to get their first academic article published. Six of the mentees ultimately were able to make submissions, and four articles from the mentees were published in 2019. Topics ranged from a review of antenatal care to perceptions of a community health worker programme. Following on from the successes of the first cohort of mentees, the Alliance teamed up with HSG and the journal Health Policy and Planning to launch a new round of mentorship in 2019. A special issue from the next cohort is expected to be launched at the Sixth Global Symposium on Health Systems Research in Dubai in 2020.
Change-maker scholarships and support to the Pre-World Health Assembly workshop
"I will utilize the networks made at this event to further understand and be even more active in the field and, most importantly, in a local capacity in order to improve communities back home with the mantra of ‘think global, act local’".
– KAPIL NARAIN, Medical Student from South Africa
and
recipient of the IFMSA Change-Maker Scholarship sponsored by the Alliance
– KAPIL NARAIN, Medical Student from South Africa
and
recipient of the IFMSA Change-Maker Scholarship sponsored by the Alliance
Opening the eyes of young medical students to the bigger picture of health policy and systems research is critical. It can help situate their future careers as medical professionals, but it can also help establish the health policy and systems researchers of the future.
To this end, in 2019 the Alliance teamed up with the International Federation of Medical Students Associations (IFMSA) to support a Pre-World Health Assembly Workshop and to ensure participation from students in LMICs through sponsoring a Change-maker Scholarship. Three scholarship recipients from South Africa, Nepal and Egypt joined the four-day workshop, which included opportunities to develop skills, gain knowledge and contribute to collective advocacy campaigns around issues discussed in that year’s World Health Assembly. The Alliance contributed to the workshop programme, presenting on HPSR, and scholarship recipients had the opportunity to meet Alliance staff in our offices in the World Health Organization headquarters.
Strengthening HPSR capacity on intersectionality & gender equity
Addressing social inequalities is essential for improving health and well-being for all
Gender and other social factors interact to influence how people are able to maintain good health and well-being around the world. Understanding how these factors intersect in individuals and communities can help inform how health policies and systems are structured.
The Alliance launched a new programme of work on gender and intersectionality for HPSR in the South East Asia Region. The Ramalingaswami Centre for Social Determinants of Health in India was selected as a lead regional mentor institute. They have launched an 18-month research fellowship programme for participants from the region, especially from fragile and conflict-affected settings. Fellows will participate in a mix of in-person and online courses, which will also serve as the basis for a global online resource on gender and intersectionality open to others beyond the initial fellows.
Heightening Institutional capacity for Government use of Health Research (HIGH-Res)
HIGH-Res will help us to focus on strengthening the institutional structures and processes needed to meet this growing requests for evidence [on realizing universal health coverage].
-Dr. CHARLES NZIOKA
Director, Directorate of Health Policy, Research,
and Monitoring and Evaluation, and Informatics
Ministry of Health, Kenya
Effective HPSR leadership is supported by strong institutions that ensure a culture of local evidence generation and use for strengthening health systems. We are testing different models for institutional strengthening, including working directly with ministries of health in three East African countries.
HIGH-Res, a three-year, US$ 1 million project co-funded with Wellcome Trust, began in August 2019. The project is implemented by a consortium of health research institutions and ministries of health in Kenya, Uganda and Malawi. It is led by the African Institute of Development Policy (AFIDEP). The project will strengthen existing institutional systems, structures and processes within the ministries of health, while introducing new ones, and integrating individual capacity strengthening to enable sustained evidence-informed decision-making. In 2019, inception activities were completed, and the team in Kenya is working to strengthen capacities within the Research and Innovation sub-committee of the UHC Committee. In Malawi, the team contributed significantly to the development of the recently launched health research policy and will support its implementation strategy.
Building Institutional Capacity for HPSR and Delivery Science (BIRD)
"We are building a cadre of policy-making and research institutions that have the right systems, processes and culture in place to champion and institutionalize the use of evidence in decision-making in health."
- FADI EL-JARDALI,
Director of the Knowledge to Policy Centre
American University of Beirut
- FADI EL-JARDALI,
Director of the Knowledge to Policy Centre
American University of Beirut
Creating an enabling environment for HPSR requires strong teaching institutions and policy institutes that can provide relevant and rigorous training in HPSR methods
and models.
The mentor institute (American University of Beirut Knowledge to Policy Centre), has been engaging six mentee institutes, one from each WHO region. Since a capacity strengthening workshop on various models of evidence-informed policy-making in May 2019, the mentor institute has run five webinars. The mentee institutes are advancing work in their home policy and research networks in priority-setting exercises, developing knowledge translation products on identified topics, producing training materials and courses, and trialling prototype policy fellowship programmes.
We advance knowledge.
One of the main ways the Alliance supports the development of HPSR is by commissioning relevant research projects that either build the field or that contribute to knowledge of a specific HPSR topic.
The Alliance works across a number of thematic areas to expand knowledge on HPSR, especially in the context of achieving UHC and the wider SDGs. In particular, we have a portfolio focused on primary health care, one on health systems barriers to achieving UHC, and continued work on migration and on immunization. One of the Alliance’s strengths is that it applies embedded research and systems thinking approaches to these topics. We also invest in building knowledge on HPSR methods

Advancing knowledge
Ethical considerations for HPSR
"Practitioners of HPSR grapple with a distinct set of ethical issues reflecting the multidisciplinary nature of the field. [...] This document shines a light on these ethical issues and offers a series of considerations for all those involved in HPSR."
— Dr SOUMYA SWAMINATHAN, Chief Scientist
World Health Organization
— Dr SOUMYA SWAMINATHAN, Chief Scientist
World Health Organization
When is a project health research and when is it health practice? Is research ethics review required for studies of existing policy decisions? These are some of the ethical conundrums HPSR researchers face as they design their studies.
Resolving these issues is not always straightforward. Research ethics committees working in public health may have more experience in biomedical and epidemiological research than in the transdisciplinary field of HPSR. This publication suggests 14 points to consider for researchers and research ethics committees when constructing HPSR studies, and it illustrates and illuminates these points using six case studies. It was one of the most downloaded documents on the Alliance website the month of its release.
Special issue of Globalization and Health
Health in the SDGs: Inter-sectoral action for health
The SDGs recognize that current challenges facing the globe are interrelated – often inextricably linked to each other. However, much work on achieving the SDGs remains in silos. Goal 3 focuses explicitly on health, however, almost all other goals are related to or contribute to health and well-being.
This 14-article collection is focused on policies and programmes outside the health sector – often in collaboration with the health sector – that have health implications through commercial, cultural, economic, environmental, political, or social determinants of health. It gathers critical lessons on effectively engaging other sectors to enhance their health outputs, identifying co-benefits and ‘win-wins’ that enhance human health.
Special issue of BMJ Global Health
Strengthening primary health care through research: Prioritized knowledge needs to achieve the promise of the Astana Declaration
Strengthening primary health care systems is a critical component to achieve UHC. And while there is increasing eagerness to build, reform and strengthen these systems in many LMICs, country leaders are often unsure where to begin.
In a sweeping new effort, this special issue gathered 76 researchers, practitioners, and policy-makers from 19 countries to identify the gaps in global knowledge about what works in primary health care and prioritize a new research agenda. Key areas of focus include: organization and models of care; quality, safety, and performance management; policy and governance; and financing of primary care systems.
Key articles from 2019
Intersectoral and integrated approaches in achieving the right to health for refugees on resettlement:
a scoping review
By Shirley Ho et al. in BMJ Open
ahpsr.org/refugees
This article is the result of a joint programme of work on migration and health with the Swedish Institute for Global Health Transformation (SIGHT), which aims to enhance the integration of refugee health services within health systems and identify research needs to advance the right to health for refugees. The scoping review explores the barriers and facilitators to the integration of health services for refugees, the processes involved and the different stakeholders engaged in leveraging intersectoral approaches to protect refugees’ right to health on resettlement. It formed the basis of a session at the Prince Mahidol Award Conference (PMAC) in January 2020.
Embedding implementation research to enhance health policy and systems: a multi-country analysis from ten settings in Latin America and the Caribbean
By Etienne Langlois et al. in Health Research Policy and Systems
ahpsr.org/eirLAC
The Alliance has a long track record of supporting embedded implementation research projects around the world. But what have we learned about the approach? An article learning from one set of these projects across in the region of the Americas was published in November. It identifies 17 facilitators and eight barriers to embedding research into policy and systems. The principal facilitating factors were actionability of findings, relevance of research and engagement of decision-makers, whereas the main barriers were time and political processes.
Conceptual framework of equity-focused implementation research for health programs (EquIR)
By J. Eslava-Schmalbach et al. in the International Journal of Equity in Health
ahpsr.org/equir
The Alliance contributed to the development of EquIR: the equity-based framework for Implementation Research of health programmes, policies and systems. EquiIR is a conceptual framework proposed for use by decision-makers and researchers during the implementation of programmes, policies or health interventions aiming to reduce or prevent the increase of existing inequities during implementation.
Articles from our early-career women researchers
Determinants of antenatal care utilisation in sub-Saharan Africa: a systematic review
by Ijeoma Nkem Okedo-Alex et al. in BMJ Open
ahpsr.org/mentee1
How local context influences access to neuropsychological rehabilitation after acquired brain injury in South Africa
by Noorjehan Joosub in BMJ Global Health
ahpsr.org/mentee2
Are formal self-care interventions for healthy people effective? A systematic review of the evidence
by Nilushka Perera and Shade Agboola in BMJ Global Health
ahpsr.org/mentee3
Sub-national perspectives on the implementation of a national community health worker programme in Gauteng Province, South Africa
by Shehnaz Munshi et al. in BMJ Global Health
ahpsr.org/mentee4
We inform policy.
Health policy and systems research is a field that aims to strengthen health systems and improve health and well-being for all. For the Alliance, this means approaching research as explicitly intended to inform policy and practice.
Many of the research projects supported by the Alliance respond to questions directly identified by policy-makers in LMICs. This embedded research model helps ensure findings from our projects are used to inform policies that can have a real impact on health systems and societies. We also support evidence synthesis platforms to ensure wider bodies of evidence are considered.

Informing policy around the world
BRAZIL
The Alliance has been undertaking a joint programme on Embedding Research for the Sustainable Development Goals (ER-SDGs) with PAHO and TDR. One of the ER-SDG teams in Brazil is working on a project that focuses on the identification of factors influencing adherence to the National Guide for Natural Delivery. Based on their research results, this team is fostering the improvement and implementation of the clinical practice guide on natural childbirth at the national level. The guide will be piloted in university hospitals
ETHIOPIA
The Alliance has established a close working relationship with the WHO Country Office and with the Ministry of Health in Ethiopia. There are currently 15 embedded research projects being established in the country in conjunction with decision-makers. The projects focus either on the government’s flagship Compassionate, Respectful and Caring Health Workforce Initiative or on health systems barriers to immunization service delivery.
INDIA
In India, we worked with the WHO country office and the South East Asia Regional Office (SEARO) to support a series of demand-driven health systems research projects to inform the early implementation of India’s new National Health Insurance Scheme (PM-JAY). Based on priorities identified by senior policy-makers within India’s National Health Authority (NHA) – the scheme’s implementing agency – and engaging the NHA throughout the research process, teams from research institutions within India carried out three studies over a six-month period. Findings were shared with the NHA leadership in late August at a meeting bringing together key programme stakeholders from national and state levels. Based on the success of these studies and responding to the national policy-makers’ request for more research, a second round of studies is planned for early 2020. The Alliance has been running similar country-led implementation research projects in Nepal and Ethiopia.
MALAYSIA
As part of our ‘Embedding Rapid Reviews in Health Systems Decision-Making’ (ERA) initiative, the team in Malaysia worked on four rapid reviews in 2019. One of the reviews has been completed on the competencies and qualification required of midwives in public primary care and community clinics. It was presented to the Director of Family Health Development Division, the Director of Nursing, and other stakeholders. Informed by this review, the Director of Nursing is interested in enhancing current training of nurses to better meet the health needs of increasingly complex maternal cases
We are committed.
Sustainable changes usually require more than a single project, are informed by a concerted effort of many individuals and organizations and happen on a scale of years not months. This is true whether they are changes in policy, in practice, in building relationships and networks and in gaining and utilizing new skills.
There are some grantees for whom the Alliance has been an important catalyst to drive change in their contexts. In this section, we zoom out to look at the bigger picture and to understand how we have contributed to change in Bosnia and Herzegovina and Nigeria.

Bosnia and Herzegovina: Supporting institutional reform
THE CHALLENGE
The Public Health Institute (PHI) of Republic of Srpska has a mandate from the Ministry of Health and Social Welfare to monitor health outcomes in the region, paying particular attention to epidemiology, health surveillance, water and food control, and generating and managing health statistics. One of its branches, the Health Management Centre (HMC), was focused on providing capacity building, carrying out services for the PHI and undertaking advisory work for the public and private sector in the country. However, the Centre had little experience undertaking research – even though there was significant interest among its staff to do so, as several of them also taught at local universities.
THE ALLIANCE’S INPUT
In 2014, the Alliance put out a call for research proposals on the role of non-state providers to move toward UHC. Staff at HMC spotted the call and put together a proposal in the hopes of kick starting its research programme.
The nature of the HMC’s work made its staff quite aware of the challenges facing the health sector in Republic of Srpska – a major one being that the majority of private health care providers failed to adopt the safety and quality standards introduced in 2012 by the Ministry of Health and Social Welfare. The HMC proposed research into the reasons why some private health care facilities were adopting the new standards while others were not, and were ultimately successful in winning a research grant from the Alliance.
Before starting work on the two-year research project, the Alliance offered the opportunity to spend time designing the project’s research protocol. This process took almost an entire year. During the protocol design phase, the HMC and seven other grantees of the Alliance worked closely with Johns Hopkins University Bloomberg School of Public Health, which had been contracted by the Alliance to provide technical support and quality control to the studies. Johns Hopkins helped the HMC with the protocol design and throughout the research process.
The HMC team used a mixed-methods approach, which was new for the HMC, and indeed for the wider PHI. Because of their limited experience with research, the support from the Alliance and Johns Hopkins was fundamental in securing local stakeholders’ acceptance of the chosen methods. The study also provided some new ideas on how evidence may be generated and used for policy-making in the Ministry.
After the research was completed in 2018, the findings were presented to the Ministry of Health, associations of private health care providers, and the union of medics, dentists and pharmacists. The fact that their results were backed by both the Alliance and Johns Hopkins University was important to assure local credibility. The results and recommendations were well received – even if they have yet to be implemented.
THE RESULT
Even if the research did not immediately lead to impact in the adoption of safety standards, it did have important consequences for the HMC, PHI and the role of evidence in policy. Although the PHI’s mandate had included the provision of policy recommendations on health systems to the Ministry of Health and Social Welfare, the HMC had not done so until 2015 with the Alliance’s grant. This project constituted the first time the HMC effectively undertook research to provide evidence-based policy recommendations.
After this experience, the PHI decided to strengthen its capacity to provide more, and better, evidence-based policy recommendations to the ministry. In 2018, it changed the mandate of the centre and it was renamed the Centre for Health System Development and International Cooperation (CHSDIC).
As a consequence, CHSDIC has turned its attention to submitting more applications for research funding. It has been successful in a recent bid from the Alliance to look at citizen-responsive insurance schemes. This has strengthened its relationship with the Ministry, having formed a joint team to design projects and submit applications.
Nigeria: Building bridges between policy-makers and researchers for evidence-based health policy
THE CHALLENGE
Dr Chigozie Jesse Uneke is a parasitologist by training and a professor from Ebonyi State University in Nigeria. He was interested in epidemiology and the diseases affecting the most vulnerable and poor, but he found that policies to tackle epidemics in rural Nigeria were often not very effective because they had not been tailored to the diversity of contexts where they were meant to be implemented.
His suspicion was that this was down to a lack of interaction between policy-makers and researchers. There was, in fact, no effective collaboration or any kind of partnership between them in Ebonyi State.
THE ALLIANCE’S INPUT
Dr Uneke and his team at the Ebonyi State University applied for and received a grant from the Alliance in 2009 to begin a process of bringing together policy-makers and researchers and to enhance the capacity of researchers to produce the kind of evidence that policy-makers required – all while showing policy-makers the advantages that evidence-informed policy could present for them and for the country.
The grant allowed them to undertake several capacity-building workshops with both policy-makers and researchers. The constant interaction between them helped participants to understand each other better. Some of the challenges that created and maintained the divide between them were addressed – mutual mistrust of their motivations being the main one. This issue was solved mainly through the friendships that developed from these constant interactions. Only after this first barrier was overcome were they able to begin working together. This led to the development of a shared research agenda that was relevant for both groups.
As a result of this first process, the Health Policy Advisory Committee was created in 2011. This committee was made up of senior policy-makers from the Ebonyi State Ministry of Health and senior researchers from Ebonyi State University who come together to tackle issues raised by its members.
A second grant from the Alliance, in 2014, helped the group to set up a digital policy information platform that offers evidence syntheses, policy briefs, policy notes and other materials relevant for health policy-making. After a series of consultations with both policy-makers and researchers, the site was launched in 2015 and continues to be active. This second grant also led to the formation of Ebonyi State University’s African Institute of Health Policy and Health Systems (AIHPS). AIHPS undertakes research and offers postgraduate degrees on health policy and systems research, as well as short training sessions and a postgraduate diploma.
This experience helped to deepen the understanding each group had of each other’s work, thus facilitating future collaboration.
THE RESULT
The Alliance’s long-term investment in these projects has helped to strengthen the relationship between policy-makers and researchers in Ebonyi state. This relationship was then consolidated in the formation of two new institutions, critical for any functioning evidence-informed health system: the Health Policy Advisory Committee and the AIHPS.
The policy information platform is both an output and an outcome of this process, as it represents the impact of the new working relationships that were developed.
These changes demonstrate a progressively nuanced and transformative change. First, new relationships were forged; they were then put into practice through the development of an advisory body and they were further institutionalized through the foundation of a new institute.
2019 finances and donors
The Alliance gratefully acknowledges the continued core financial support from the Norwegian Agency for Development Cooperation (Norad), the Swedish International Development Cooperation Agency (Sida), and the United Kingdom of Great Britain and Northern Ireland Department for International Development (DFID).
Other donors and those supporting ongoing activities in 2019 include the Doris Duke Charitable Foundation, Gavi, the Vaccine Alliance, the International Development Research Centre, Canada (IDRC), UNICEF, the UN Foundation, the United States Agency for International Development (USAID) and Wellcome Trust.
Governing bodies
Alliance Board
CHAIR David H. Peters, Professor and Chair, Department of International Health, Bloomberg School of Public Health, Johns Hopkins University, United States of America
Gail Andrews, Chief Operating Officer,
National Department for Health, South Africa
Keshav Desiraju, Former Union Health Secretary, Government of India, India
Dirk H. Mueller, Senior Health Adviser, Health Research Team, Research and Evidence Division, Department for International Development (DFID), United Kingdom
Kelechi Ohiri, Chief Executive Officer, Health Strategy and Delivery Foundation, Nigeria
Ingvar Theo Olsen, Policy Director, Department for Global Health, Education and Research, Norwegian Agency for Development, Norway
Walaiporn Patcharanarumol, Director, International Health Policy Programme, Ministry of Public Health, Thailand
Teresa Soop, Senior Research Advisor, Swedish International Development Cooperation Agency (Sida), Sweden
Soumya Swaminathan, Chief Scientist, World Health Organization, Switzerland
Naoko Yamamoto, Assistant Director-General, Universal Health Coverage and Health Systems, World Health Organization, Switzerland
Scientific and Technical Advisory Committees
CHAIR Jeanette Vega, Chief Medical Innovation and Technology Officer, Red de Salud UC CHRISTUS, Chile
Trish Greenhalgh, Professor of Primary Care Health Sciences, Nuffield Department of Primary Care Health Sciences, University of Oxford, United Kingdom
George Pariyo, Senior Scientist, Department of International Health, Bloomberg School of Public Health, Johns Hopkins University, United States of America
Sabina Faiz Rashid, Dean and Professor, James P Grant School of Public Health, BRAC University, Bangladesh
Emma Sacks, Associate Faculty, Department of International Health, Bloomberg School of Public Health, Johns Hopkins University, United States of America
Helen Schneider, Professor, School of Public Health, University of the Western Cape, South Africa
Göran Tomson, Professor, Karolinksa Institutet; Senior Advisor, Swedish Institute for Global Health Transformation (SIGHT), Royal Swedish Academy of Sciences, Sweden
Alliance Secretariat
Abdul Ghaffar, Executive Director
Kabir Sheikh, Policy Advisor
Oyetayo Akala, Young Professional (Health Systems Research)
Priscilla Cleland, Administrative Assistant
Karen Daniels, Technical Officer
Marta Feletto, Technical Officer
Dena Javadi, Technical Officer
Gloria Kelly, Programme Officer
Jeff Knezovich, Technical Officer, Partnerships and Engagement
Aku Kwamie, Technical Officer
Etienne Langlois, Technical Officer
Zubin Shroff, Technical Officer
John Warriner, Technical Officer
NOTE: People listed on this page served on the Board or STAC or were employed by the Secretariat at some point during 2019. They do not necessarily reflect the current composition of these bodies.
© World Health Organization 2020
Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo.
Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization .
Suggested citation. 2019 annual report of the Alliance for Health Policy and Systems Research. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO.
Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris.
Sales, rights and licensing. To purchase WHO publications, see http://apps.who.int/bookorders. To submit requests for commercial use and queries on rights and licensing, see http://www.who.int/about/licensing.
Third-party materials. If you wish to reuse material from this work that is attributed to a third party, such as tables, figures or images, it is your responsibility to determine whether permission is needed for that reuse and to obtain permission from the copyright holder. The risk of claims resulting from infringement of any third-party-owned component in the work rests solely with the user
General disclaimers. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of WHO concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by WHO in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters.
All reasonable precautions have been taken by WHO to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall WHO be liable for damages arising from its use .
Design and layout by Michelle Samplin-Salgado, Miami Beach, FL, United States.
Printed by the WHO Document Production Services, Geneva, Switzerland.